Learnings from the Maldives’ Declining Maternal Mortality Rates

“Maternal mortality health is a very sensitive indicator. All you need to look at is a country’s maternal mortality rate. That is a surrogate for whether the country’s health system is functioning. If it works for women, I’m sure it will work for men.” – Margaret Chan
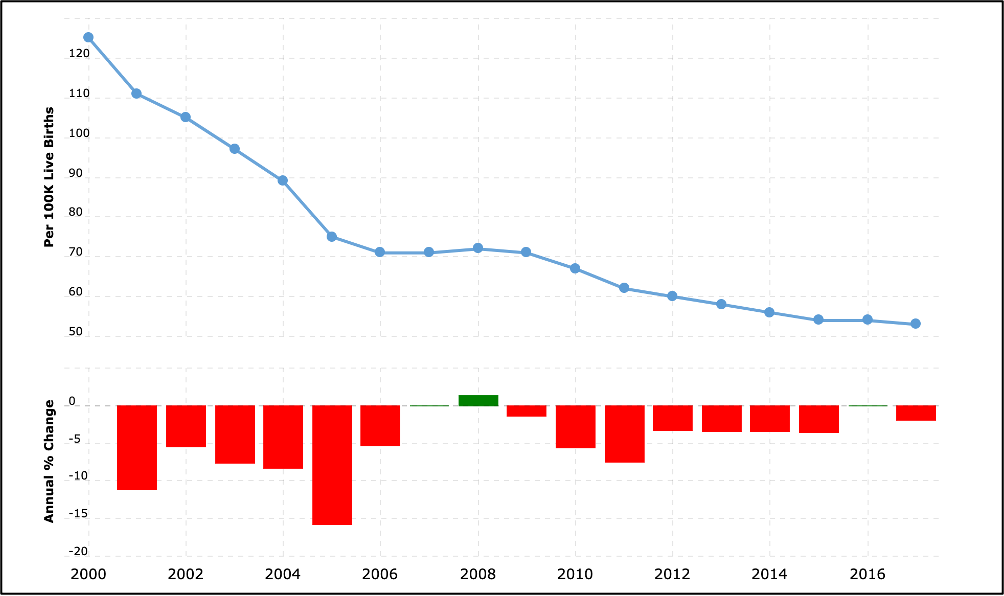
The Maldives has focused on improving its health system over the last couple of decades. Consequently, according to World Bank estimates, there has been a stunning 136 percent plunge in its maternal death rate from 2000 to 2017 – one of the most significant drops in the world over this period. In 2000, out of every 100,000 live births, 125 women died of pregnancy-related causes. In 2017, that number decreased to 53, which occurred during a time of modest annual growth in income (just over 2 percent per year on average). However, the world saw a much smaller annual decline in the maternal mortality rate around the same time. Thus, the Maldives is an exemplar when it comes to reducing maternal deaths. So, what can other resource-constrained countries learn from the Maldives around strategies to reduce maternal mortality rates?
Two decades ago, the Maldives faced enormous hurdles when delivering maternal health care. For one thing, its residents are spread across 187 islands, and only four islands have more than 5,000 inhabitants. On top of that, the country’s health system was underdeveloped, with only a few regional hospitals providing emergency obstetric care. As a result, maternal death rates were at concerning levels. The most recent research by the World Health Organization (WHO) gives insight into the various tactics employed by the Maldivian government to address the maternal mortality crisis. First, the health ministry introduced an in-depth review process that assessed the specific causes of all maternal deaths, helping health officials understand why women were dying and how to prevent it. Furthermore, healthcare workers received additional training and were deployed to provide necessary home visits. Close monitoring facilitated by the home visits proved to be essential, particularly for women with high-risk pregnancies. Finally, the government collaborated with health officials to make emergency obstetric care available to all women within two hours of travel – no matter where they were – by expanding the healthcare system and individual healthcare facilities. As a result, more than 95% of births are now attended by skilled medical staff.
The rapid increase in the number of nurses and midwives has been significant, from the low single digits per thousand people to more than eight per thousand people. This is more than four times the average in South Asia and comparable to many countries across Europe. Equally noteworthy have been the interventions and policies geared towards nutrition; all pregnant women receive appropriate supplements, such as iron and folic acid, at antenatal appointments. Taking the right supplements has reduced nutritional deficiencies, which are a crucial contributor to conditions like anemia – a complication that is prevalent in pregnant women. However, because of the health measures put in place, the share of women of reproductive age with anemia fell dramatically.
At the same time, access to family planning information was improved, in order to educate parents about the importance of planned pregnancies. During home visits, community health workers informed women about the benefits of contraceptives, such as saving lives by preventing unintended pregnancies, reducing the number of abortions, and lowering pregnancy-related deaths and disabilities. The government also increased the number of contraceptive products available, including male and female condoms, oral contraceptives, intrauterine devices, and implants. Furthermore, the government raised awareness about the importance of overall reproductive health care. Dramas and songs about all aspects of reproductive health – from contraception and conception to maternal nutrition and safe delivery – were disseminated through mass media. Today, all of the hospitals in the Maldives have emergency obstetric care facilities, and nearly every birth takes place in a healthcare facility.
While the Maldives has made significant progress in reducing the maternal mortality rate, numerous issues have yet to be solved. For example, health staff shortages remain a critical concern because specialist services are dependent on foreign professionals, leaving the health system vulnerable to their departure. In addition, sexual and reproductive health services are primarily directed toward couples, making it difficult for young, unmarried people to access contraceptives and reproductive health information. With complications from abortion and the recent decline in contraceptive prevalence, the Maldives government is now turning its attention to young people by advocating for sex education in schools and encouraging policies to provide reproductive health awareness to younger individuals.
In summary, the Maldives provides a fantastic blueprint of a strong healthcare infrastructure for many countries, particularly those with limited resources, such as the Bahamas, Tonga, Guyana, Northern Ireland, and others. Active government involvement coupled with a data-driven approach focused on constant measurement and improvement is the key to a sustained reduction in the maternal mortality rate.
Sources:
https://ourworldindata.org/hannahexemplar
https://www.unfpa.org/news/stunning-plunge-maternal-deaths-recorded-maldives
https://www.macrotrends.net/countries/MDV/maldives/maternal-mortality-rate
https://www.nature.com/articles/s41598-021-97481-3